Revenue Cycle Management: Why Agentic AI is the answer to $140 Billion in waste

Moveo AI Team
16 de janeiro de 2026
in
Percepções da liderança
In the current healthcare macroeconomic landscape, clinical excellence has become only one part of the sustainability equation. The other half, often underestimated until it becomes a crisis, is the organization's financial health. At the center of this battle lies Revenue Cycle Management (RCM).
For decades, revenue cycle management was treated as a purely operational back-office function. Today, it has ascended to the strategic agenda of administrative boards.
The reason is purely mathematical: according to McKinsey research, health systems collectively spend more than $140 billion annually on manual processes and fragmented technologies. The typical RCM process consumes 3% to 4% of a health system's net revenue at scale.
We are, however, facing a paradigm shift. The era of automation based on simple scripts is over. We are entering the era of Agentic AI, a technological evolution that promises to unlock the first credible path to a truly "touchless" revenue cycle (one without human intervention) and reduce the cost-to-collect by 30 to 60 percent.
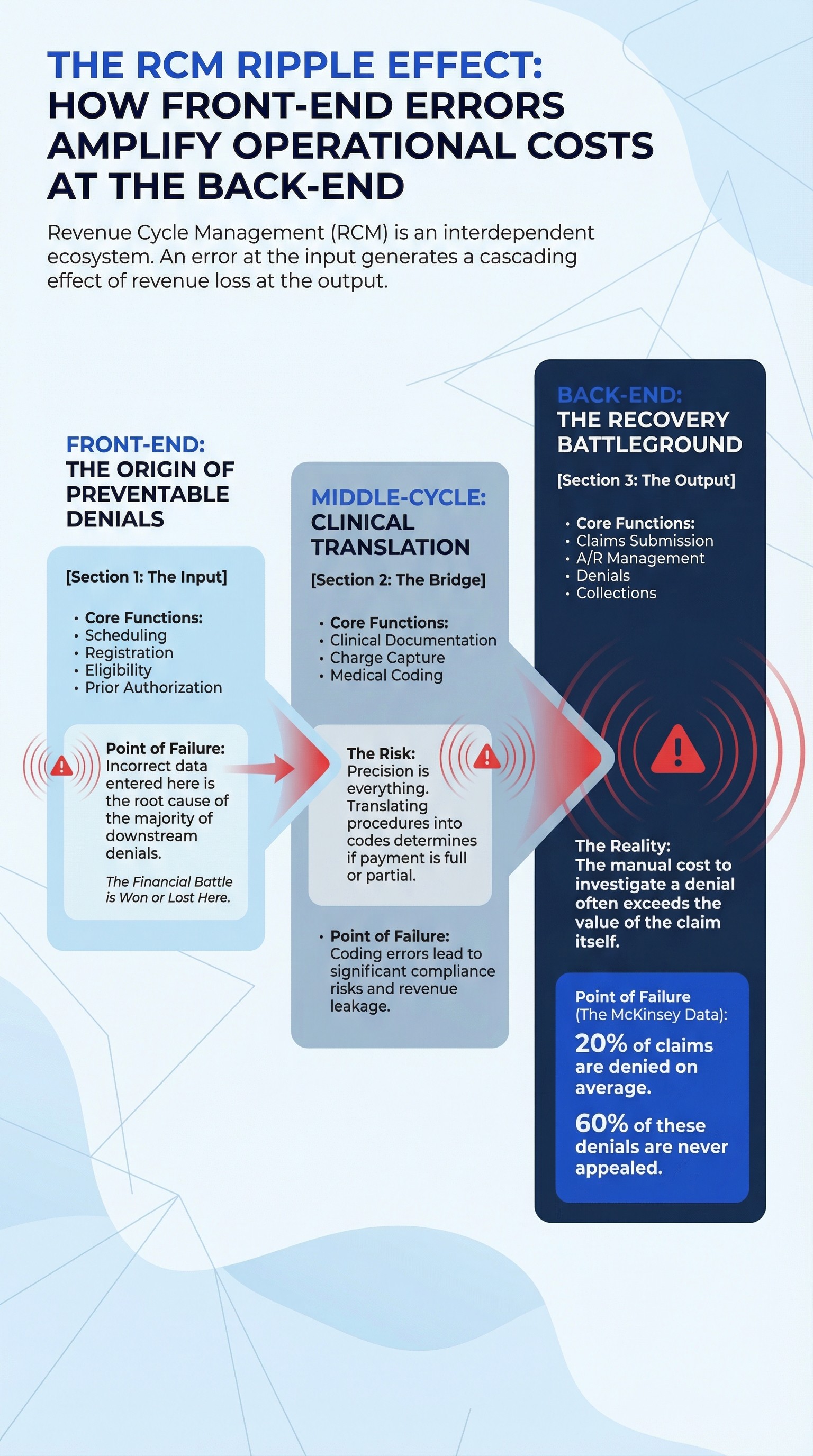
Before we understand Agentic AI, we must first grasp the complexity of the current cycle. RCM is not monolithic, it is an ecosystem of interdependent functions where an error at the input generates a cascading effect of loss at the output.
Imagine the cycle as a high-precision industrial production line, divided into three critical stages:
1. Front-End: The Origin of "Preventable Denials"
The cycle begins long before the clinical encounter. It is in this Patient Access phase that the financial battle is often won or lost.
Critical Components: Scheduling, Registration, Eligibility Verification, and Prior Authorization.
Point of Failure: This is the most critical stage. Incorrect data entered here is the root cause of the majority of downstream denials. The complexity of health plans and the lack of real-time integration turn prior authorization into a massive administrative bottleneck.
2. Middle-Cycle: Clinical Translation
This is the bridge between medical care and billing.
Critical Components: Clinical documentation, charge capture, and medical coding.
Point of Failure: This is where medicine meets bureaucracy. Precision in translating a clinical procedure into a code (such as ICD or CPT) defines whether payment will be full or partial. Coding errors generate significant financial and compliance risks.
3. Back-End: The Recovery Battleground
Where financial execution takes place.
Critical Components: Claims submission, accounts receivable (A/R) management, denials management, and collections.
Point of Failure: This is where cash gets stuck. Currently, about 20% of claims are denied by payers. The most alarming data from McKinsey reveals that 60% of these denials are never appealed. Why? Because the manual cost to investigate and appeal the denial often exceeds the recovered value.
Revenue Cycle Management Challenges: Why Traditional Automation Failed
If RCM is so critical, a difficult question must be asked: If billions have been invested in RPA (Robotic Process Automation) over the last decade, why is the industry still bleeding $140 billion annually in inefficiencies?
Persistent revenue cycle management challenges stem from the nature of legacy tools. Traditional RPA excels at rigid, repetitive tasks but breaks when confronted with variability.
If a payer portal moves a button, the bot stops.
If a denial requires clinical interpretation of unstructured medical records, the bot fails.
The result is a fragmented process where humans act as "glue" between systems, performing low-value tasks while strategic intelligence is consumed by bureaucracy. This leads us to unsustainable metrics, such as a stagnant cost-to-collect at 3-4% of net revenue and a chronic shortage of medical coders and analysts.
Learn more→ US Delinquency Landscape 2026: Credit Duality and the Role of Agentic AI
A change of course? What the data says (2023 vs 2025)
Healthcare sector leaders are reacting. Recent McKinsey data reveals a drastic shift in technological investment intentions. The search for point solutions is giving way to a demand for integrated, intelligent platforms.
The table below illustrates where RCM leaders are allocating their political and financial capital:
RCM Function | Priority in 2023 | Priority in 2024 | Priority in 2025 (Projected) | Trend |
Prior Authorization (Front-end) | 35% | 44% | 60% | Accelerated Growth |
Coding (Middle-cycle) | 37% | 39% | 51% | Constant Growth |
Denials or Appeals (Back-end) | 39% | 23%* | 61% | Aggressive Resurgence |
Accounts Receivable Follow-up | 22% | 24% | 26% | Stability |
Source: McKinsey & Company, "Agentic AI and the race to a touchless revenue cycle"
Observe the jump in Denials or Appeals, reaching 61% prioritization intent in 2025. This signals that the market has recognized that "revenue leakage" at the back-end is the most urgent problem to staunch.
The Back-End as the ignition point
The data above confirms a clear trend. Although the ultimate vision is an autonomous end-to-end cycle, the most prudent and effective strategy to begin this journey is to focus on the back-end of the revenue cycle.
Why start at the end?
Safety and Low Risk: The back-end is largely administrative. Unlike the front-end, which involves direct interaction with the patient, or the middle-cycle, which touches on clinical decision-making, the back-end is a controlled environment.
Ideal for Agentic AI Automation: Functions such as A/R follow-up, underpayment management, and cash posting are governed by clear rules and repetitive patterns. This allows AI to learn and replicate work with high fidelity.
Resource Liberation: Automating these high-volume tasks frees the team to manage complex exceptions, increasing organizational productivity.
Migration to a Hybrid and "Touchless" operating model
We are not talking about a distant future. Agentic AI is operating today in revenue recovery, transforming the operating model.
Unlike Generative AI (which merely offers advice), Agentic AI executes recovery. Consider a use case in Denials Management:
The Problem: A payer denies a batch of claims alleging "lack of clinical justification". A human would take hours to download each medical record, write individual letters, and upload them.
The Agentic Solution: The AI agent detects the denial. It autonomously enters the system (EHR), reads the unstructured medical record, identifies the clinical evidence, drafts the specific appeal letter for that case, logs into the payer portal, and submits the appeal.
The Result: The cycle is closed in minutes, not weeks. The human intervenes only if the Agent signals a complex exception.
In this model, Agentic AI allows analysts to stop being paper processors and become revenue strategists.
The ROI of transformation
The final argument for adopting Agentic AI is not technological, it is financial. If successfully implemented, a "touchless" RCM engine can deliver transformational value.
Projections indicate that enabling the revenue cycle with AI can lead to a 30 to 60 percent reduction in cost-to-collect.
Let's translate this into real numbers: For a health system with patient revenue in the range of $6 billion, reducing the cost-to-collect by just 1 to 2 percentage points (thanks to agentic automation) would result in direct savings of $60 million to $120 million annually.
Beyond direct savings, there is an intangible but critical gain: the redirection of the workforce. As AI agents take on heavy, repetitive work, the human team can be refocused on high-value activities centered on patient experience and resolving complex cases.
Transforming the Back-End into a value engine
The healthcare industry has awaited a structural change in RCM performance for decades. With Agentic AI, that change is no longer a distant promise—it has become a tangible operational capability.
Moving the revenue cycle from a fragmented, reactive process to an intelligent, adaptive system represents an inflection point. Organizations that act now to integrate autonomous agents, starting strategically with the back-end, will not only solve their revenue cycle management challenges but will define the new standard for financial efficiency in the sector.
The question for healthcare leaders in 2026 is not if AI will manage your revenue cycle, but how fast you can empower it to do so.
Want to know how to apply this to your operation?
Moveo is at the forefront of Agentic AI. If you wish to understand how our autonomous agents can be deployed specifically within your Denials Management workflow to capture lost revenue, contact our experts →
